The importance of eye and ear health
by stories by Marc Huminilowycz
photography by Jessica Crandlemire

Listening to inspiring music; taking part in a stimulating conversation; enjoying a movie; seeing a smile on a friendly face; watching children or grandchildren grow; taking in the wonderful sights and sounds of life around us – of our five senses, vision and hearing are arguably the most integral to our daily lives and the way in which we interact and communicate with the world. Yet most of us take these senses for granted until we notice problems with them.
I have personally been reminded of the importance of eye and ear health – and the fact that you don’t have to be “old” to experience sight and hearing issues. Eight years ago, at age 57, I had a wake-up call that my vision was poor.
After noticing – and ignoring – a slight darkening in my vision for a number of years (as though someone had put a brownish lens over my left eye), I finally had a wake-up call when I backed up my car in an underground parking lot in Toronto and hit a post that I didn’t see.
I went to my family doctor, who referred me to an opthamologist. Tests showed that I had a cataract on my left eye. I had surgery to replace the damaged lens with an artificial one – a surprisingly quick, simple and painless procedure these days – and within an hour I was walking around, marvelling at my ability to see clearly for the first time in years. Everything was brighter and more defined, and I have had no further problems since. My only regret is that I didn’t get my eyes checked sooner.
I have also experienced moderate hearing loss due to a couple of factors. Likely caused by playing in a very loud rock band in my youth, I have some nerve damage in my inner ear that makes it difficult to hear middle to upper frequencies (I can understand male voices better than female voices and adults better than children, for example). I also have bony (benign) growths in both of my ears that have almost completely blocked my ear canals.
The latter is actually a recurrence of a condition that I experienced in my 20s, called “exostosis.” Commonly known as “swimmer’s ear’ or “surfer’s ear,” it is believed to be caused by swimming in cold water without ear protection. When I was originally diagnosed, an ear nose and throat specialist recommended surgery to remove the bony growths, called exostoses, from my ear canals. The procedure was a success, and my hearing improved.
For whatever reason, the exostoses have grown back later in life. Aggravated by the nerve damage in my inner ear, which has been confirmed by auditory testing, my hearing loss is now forcing me to turn up the volume on the phone, TV and stereo, to frequently ask people during conversations (including my very patient wife) to repeat parts of what they say, and to miss portions of conversations in social situations entirely.
A couple of months ago, as a result of a nasty cold and ear congestion, it became even more difficult for me to clearly hear conversations on the phone or in a crowded space, or to watch TV without turning up the volume to an annoying level.
I recently saw Dr. Sumit Agrawal, an otolaryngologist and neurotologist (head and neck surgeon) at University Hospital in London, Ontario for an opinion on whether or not removing my exostoses will improve my hearing. Dr. Agrawal advised that surgery – on my right ear only, which is more blocked than the left – may or may not improve my hearing, but will at least help to unblock the ear canal and prevent future ear infections.
Perhaps, like many of us as we get older, I was in denial about my hearing loss and the unacceptable notion that it could be the result of aging. But given the relatively simple nature of the procedure (day surgery) and the prospect of possibly hearing better afterwards, I have decided to proceed with the operation. Ultimately, I may also have to consider getting fitted for a hearing aid.
I was referred to Dr. Agrawal by my ear, nose and throat (ENT) specialist, Dr. Alexander Marsh, who had been seeing me about my hearing at his Owen Sound office for several years. Now retired, Dr. Marsh has treated hundreds of patients for a variety of auditory conditions during his practice.
He explains that moderate “swimmer’s ear,” usually caused by a simple infection, is a condition experienced by up to 15 per cent of the population. Only a small fraction of patients, like me, may require surgery to correct the problem. “Simply put, your exostoses will be drilled off, and the ear canal should heal within two weeks,” he says. “Following the surgery, it is very important to keep the ear canal dry and free of contamination, and avoid any pressurization of the ear (excessive nose blowing) or physical straining.”
Dr. Marsh describes hearing loss as falling under two primary categories: conductive and nerve. Conductive hearing loss occurs when sound going into the ear is blocked due to problems in the ear canal, the eardrum or the middle ear and its delicate components. It is typically caused by an infection, excessive wax build-up, a perforated eardrum, allergies, fluid in the inner ear or a benign tumour. In most cases, conductive hearing loss can be corrected with medication, surgery or therapies. Nerve hearing loss (as I have) is caused by damage in the inner ear and/or the auditory nerve. It can only be corrected with an assistive hearing device.
“In my practice, the most common hearing problem was conductive hearing loss among children,” Dr. Marsh observes. “An infection causes a build-up of fluid in the middle ear, which sometimes doesn’t go away, or the eustachian tubes don’t ventilate properly. The problem can be long-term in children, but usually clears up by the time they are eight to 10 years old. This can be an issue among adults as well.”
Indeed, hearing problems are not necessarily age-related, notes Dr. Marsh. In his years of practice, he treated patients from infancy through to age 90-plus.
Collingwood resident Lynn Molyneux has had hearing problems for a number of years. Following a long career in emergency nursing, from which she had to retire because of her hearing, she took on a position managing Telehealth Ontario. “Wearing a headset in my left ear to talk with callers daily, I began to notice that my perception of low tones was severely diminished, even after adjusting the volume on the headset,” Molyneux recalls. “It was then that I decided that it was about time I got my hearing checked.”
Audiology testing revealed that Molyneux had moderate to severe low tone hearing loss in her left ear. In 2010, she was fitted with a hearing instrument at the Collingwood Hearing Clinic. Her first hearing aid was a small device manufactured by Starkey, which fit discreetly into her ear canal, automatically adjusting itself for noises and the environment around her.
“The clinic staff gave me a wonderful fitting,” she says. “They were very knowledgeable and helpful, working with my hearing instrument until it was just right for me. We went outside to do a test, and it was the first time I actually heard birds singing in a long time!”
Molyneux now has devices in both of her ears. “I recommend getting a hearing device sooner than later,” she says. “Your brain adapts and relearns. It’s a continuous process, like tune-ups for your car.”
Our region boasts a relatively large number of audiology clinics, which offer testing, counselling, hearing device fitting, maintenance and repairs. Hearing devices are not always necessary, but when they are, they are much improved over the obvious and uncomfortable hearing aids of old.
“Technology has changed dramatically over the years. Everything is now wireless and very sophisticated,” says Sue Vermeulen, owner and hearing instrument specialist at the Collingwood Hearing Clinic and Wasaga Hearing Clinic. “Today’s hearing instruments come in a wide variety of styles and functions depending on the type of hearing loss you have, your manual dexterity and of course, your budget.”
Ontario’s Assistive Devices program pays seniors up to $500 per year for their devices, and most health plans cover a portion of the purchase. “Because there is no one product that is suitable for everyone, we carry devices from the world’s largest manufacturers including behind the ear, in-ear, in-canal, invisible, tinnitus and wireless accessories,” says Vermeulen. Her clinics also offer a variety of assistive hearing appliances, such as TV and phone amplifiers and “Alert Master,” which connects to lights in the home to notify occupants of a ringing doorbell, phone, or other day-to-day household occurrences.
When is it time to see a hearing professional? A simple test at the end of this article will help you determine whether or not you have a hearing problem. If you think you do, the first healthcare provider to see should be your family doctor, who will likely refer you to an audiologist or an ear, nose and throat (ENT) specialist.
One such hearing professional is Mark Neukom of Blue Mountain Audiology in Thornbury who, as a licensed audiologist, is qualified to assess, treat and rehabilitate the auditory system. He can also refer patients to an ear, nose and throat (ENT) specialist, if necessary.
“At the age of 18, our hearing is at its optimum, and it slowly deteriorates from then on,” Neukom explains. “The ability to push aside our sound filtering system – a cognitive process that removes unnecessary sounds from the environment – diminishes with age. Many people start noticing that they have hearing problems as early as in their 40s. They’re having difficulty following a conversation in a busy restaurant, listening to music or watching TV.”
Neukom concedes that there is a stigma attached to hearing loss. “There’s the negative association with our grandparents’ bulky and ugly hearing aids, and there’s also the high perceived cost of hearing devices,” he says. “Loss of hearing makes people come to terms with the fact that they’re aging. I tell my patients not to be concerned about it, but to treat it the same as getting a joint replacement to improve their lives. The technology in today’s hearing devices has come a long way, with huge improvements in sound quality, processing speed and device size.”
Neukom takes a holistic approach to his audiology assessment and treatment process. “First, we find out who you are. We review your lifestyle and work history to determine issues that may be affecting your life, as well as past or current health problems,” he explains. “Genetics, diseases such diabetes, high blood pressure, and the use of certain pharmaceuticals can all impact hearing. The next step is to do a full assessment of your ears. We check your ear canals for ear wax and bony growths, the eardrum for perforation, and the middle ear for conductive hearing loss and possible arthritis or deterioration of the three small ear bones inside.”
Following the assessment, a series of hearing tests is conducted: Pure Tone Audiometry to check hearing thresholds for tones; Speech Audiometry for discrimination of single-syllable words typically used in conversations; a Bone Conduction Test to check what is going on in the auditory system and corroborate tone/speech headphone results; and an Acoustic Reflex Test to check the response of a muscle in the middle ear to loud sounds, which can cause sudden hearing loss in one ear, as well as headaches and dizziness.
Testing concludes with a discussion about treatment options. “We ask patients what they expect we can provide for them,” says Neukom. “Their response will guide our next steps. Hearing aids are only one option. There are other things available, such as auditory training and exercises, apps for smart phones and a wide variety of personal sound amplification products.”
Neucom emphasizes that hearing aids, although sophisticated and effective, do not repair hearing. “They allow what you have left to work better, and thereby lead a much more enjoyable life.” He also stresses the importance of having ears checked sooner than later – at least at age 50 – to avoid other possible (but yet unproven) complications of hearing loss such as memory loss, difficulty concentrating, fatigue and even brain shrinkage.
In addition to our five senses, some ear and eye specialists suggest that the brain itself could be considered a sixth sense, interpreting auditory and visual input as sound, pitch, colour and light. Fortunately for us, most ear issues can be successfully treated, preventing total deafness. It is not so simple with vision, however.
Phil Stevenson, former co-owner of the Creemore Echo newspaper and now retired in Collingwood, has what he calls “a perfect storm” of eye diseases: age-related macular degeneration (AMD), glaucoma and cataracts. “I was diagnosed with wet AMD in my left eye about 15 years ago,” he recalls. “At the time, I was told that there was not much that could be done for the disease. I tried various experimental treatments, but nothing helped. Then I started taking Avastin, a drug developed to treat colorectal cancer. This drug helped my eye somewhat, but the treatment came too late. Years later, when my other eye started going, I was put on injections of a new drug, Lucentis, which saved it.”
Although he acknowledges that his regular injections of the drug are not a cure, and that his eye will eventually degrade, he is thankful to still be able to read and drive a car. “I have learned to adapt to a two-dimensional world, training my brain to calculate distances.”
As to the cataract in his eye, which is moderate right now, Stevenson is hesitant to have surgery, fearing the risk, albeit small, of losing his vision entirely. And his glaucoma is being successfully managed with laser treatments and eye drops. Despite his visual impairments, Stevenson is optimistic that new treatments for his most serious disease, AMD, such as stem cell therapy, are on the horizon.
Unfortunately for another Collingwood resident, a cataract diagnosis by an ophthalmologist and cataract surgery at the relatively young age of 39 led to the later discovery of a rare and serious eye disease, retinitis pigmentosa (RP), which affects the retina’s ability to respond to light, causing a gradual loss of vision. Kevin Seaboyer, formerly in the military and now working from home on his computer as an inbound customer service representative, is legally blind and facing an uncertain future from the disease, which is, at this time, progressive and incurable.
“My straight-ahead vision is okay right now, but I have trouble with my peripheral vision, night vision and certain colours that are not the dominant colours of a prism,” says Seaboyer. To compensate for his disease and help him work, he needs the safe and familiar environment with proper lighting that his home provides.
While he never leaves his home at night, Seaboyer is far from being completely housebound, keeping busy and active by volunteering for annual Ride for Sight and Cycle for Sight events in Collingwood, and riding his bicycle around town in the daytime. As a client of the CNIB, he also takes advantage of occasional bus trips in the region.
Seaboyer remains undeterred by the prognosis and limitations of his disease. Once a year, he visits the Georgian Bay Optometry Clinic in Wasaga Beach to check the condition of his RP, receive maintenance and find out about any new treatments.
One such treatment, currently in clinical trials, shows promise. “Encapsulated therapy” involves the injection in the eye of a time-released capsule containing nutrients required to keep it healthy. “Providing my eyesight stays the same for a while, I’m confident that in the next 20 years, the discovery of different strains of RP will lead to a better understanding and treatment of my disease,” says Seaboyer.
While retinitis pigmentosa is relatively rare, age-related macular degeneration (AMD) is the leading cause of vision loss in Canada, according to the Canadian National Institute for the Blind (CNIB), affecting one million people. It is a progressive eye disease that affects central vision. People who have AMD may no longer be able to read, drive or see the faces of their family members.
Dr. Jayne Cation, an optometrist practicing in Collingwood, confirms that AMD is the most common eye disease in Southern Georgian Bay. In addition to being age related, AMD has a genetic component, and can occur at an earlier age as a result of sun exposure, poor diet or smoking.
“There are two types of AMD: dry and wet,” explains Dr. Cation. “Unfortunately, there is little that can be done for the dry version, except to slow down the disease by eating a high-antioxidant diet, taking eye supplements such as Vitalux, and wearing sunglasses. Wet AMD can be successfully treated and even reversed with injections of new ‘anti-VEGF’ drugs such as Lucentis and Eylea, which are also being used to treat a less common disease, diabetic retinopathy. The sooner either disease is diagnosed and treatment started, the better.”
In addition to AMD, Dr. Cation says cataract disease is prevalent in the region, with cataract surgery being one of the most common procedures in North America. A cataract is a clouding of the eye’s natural lens, which lies behind the iris and the pupil. “Although a cataract is mostly age related, it can also happen as a result of sun damage, heredity, injury or certain medications, says Dr. Cation. “Fortunately, cataract surgery is relatively safe, painless, quick and effective, and the outcome will, with simple laser touch-ups every few years, last a lifetime.”
As to other eye ailments, Dr. Cation notes that glaucoma – a “silent” disease of the optic nerve associated with higher pressures in the eyes, which can lead to a progressive loss of peripheral vision – is not common in Southern Georgian Bay. “Although there are different kinds of glaucoma, the disease is usually very treatable with diligent application of eye drops to lower eye pressures,” she says.
Dr. Cation stresses the importance of having your eyes checked regularly – even if your vision seems normal. “As we age, it’s common for most people to lose the ability to see up close. But with eye diseases, you can’t always feel what’s going on – like pressure, bleeding or other symptoms,” she cautions. “Often you won’t notice a problem until your vision is really bad, and by then it might be too late.”
How often should we have our eyes examined? Dr. Cation recommends that people over 65, children and diabetics see their optometrist annually; others every second year. “If you are experiencing flashes, ‘floaters,’ blurriness or loss of peripheral vision, see your eye doctor right away,” she advises.
Although I have personally experienced eye and ear issues over the past years, I am fortunate that these conditions are treatable and manageable, allowing me to continue enjoying the wonderful sights and sounds of Southern Georgian Bay. If there is one thing I’ve learned, it is that eyesight and hearing should never be taken for granted. In addition to protecting these precious senses, it is important to have them checked on a regular basis for signs of potential problems down the road. ❧
Test Your Hearing
Here’s a simple test to see how well you’re hearing, courtesy of the American Academy of Otolaryngology.
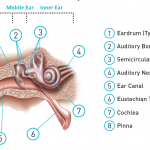
The Ear Explained
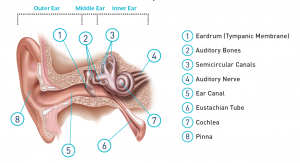 The ear is made up of three sections – the outer ear, the middle ear, and the inner ear – all working together to allow hearing and the processing of sounds.
The ear is made up of three sections – the outer ear, the middle ear, and the inner ear – all working together to allow hearing and the processing of sounds.
- The outer ear (pinna) picks up sound waves and directs them into the ear canal.
- Sound waves travel down the ear canal and hit the eardrum, causing it to vibrate.
- This vibration moves three tiny bones in your middle ear (an air-filled space between the eardrum and the inner ear) — the hammer (malleus), anvil (incus), and stirrup (stapes). The movement of these bones transmits and amplifies sound waves toward the inner ear.
- The stirrup (stapes) interfaces with fluid that fills the hearing portion of the inner ear, the cochlea, which is lined with cells covered with thousands of tiny hairs on their surfaces. As the fluid wave travels through the cochlea, it causes the tiny hairs to move.
- The hairs change the mechanical wave into nerve signals.
- Nerve signals are transmitted to your brain, which interprets the sound.
Is it Covered?
 OHIP covers some tests and devices in some cases; in others your private insurance may offer coverage or you may have to pay out of pocket. According to the OHIP website, here is what provincial health coverage provides:
OHIP covers some tests and devices in some cases; in others your private insurance may offer coverage or you may have to pay out of pocket. According to the OHIP website, here is what provincial health coverage provides:
Hearing Test
A “hearing assessment” by an audiologist in a private hearing clinic is not covered by OHIP (typical cost is $90 – $100). However, if you see your doctor and he/she refers you to an ear, nose & throat specialist (otolaryngologist), your hearing will be tested and OHIP covers this.
Hearing Aids
OHIP’s Assistive Device Program (ADP) will pay a “registered vendor” — an audiologist or a hearing instrument practitioner registered with the ADP — up to $500 per hearing device. This is available every five years unless there is a significant change in hearing. The registered vendor will fill out the ADP application for you.
Optometrist
OHIP pays for annual eye exams for people 19 or under, and those over 65. Individuals 20-64 are not covered for the $95 eye exam fee unless they have one of eight eye conditions (such as glaucoma, AMD, cataract or other eye disease) diagnosed by an optometrist.
For more information, go to www.health.gov.on.ca.
Specific information can be found at:
www.health.gov.on.ca/en/public/publications/ohip/eyecare.aspx
www.health.gov.on.ca/en/pro/programs/ohip/bulletins/4369/bul4369fs.aspx
www.health.gov.on.ca/en/public/programs/adp/publications/docs/hearaid.pdf
Help for the Visually Impaired
The Canadian National Institute for the Blind (CNIB) is a voluntary, non-profit rehabilitation agency that helps Canadians who are blind or visually impaired to overcome the challenges of vision loss and lead full, active lives.
CNIB services include rehabilitation and support, a wide range of helpful vision aid products, the latest technology (available online) to make life with vision loss easier, and one of the world’s largest libraries for people who are unable to read traditional print.
Whether you are looking for emotional support, practical ways to stay active and independent with vision loss, or more information about your vision health, the CNIB can help.
Visit cnib.ca, drop in or call your nearest CNIB office to find out more.
CNIB Owen Sound
908 2nd Ave. East, Suite 202
519-371-2721
CNIB Barrie
20 Anne St. South
705-728-3352